The NDSS is administered by Diabetes Australia
Menu
- /
- Living independently
Becoming more independent and getting your own place is a real milestone in life. When you live with type 1 diabetes, moving out of home is another big step to becoming fully responsible for your own health and diabetes management. But you won’t be alone.
Your diabetes health professionals will still be your best information source. And we’ve got you covered with tips to help you as you take charge of living your best life with diabetes.
There’ll be more to organise and plan for, like doing your own shopping and cooking, booking your medical appointments and ordering diabetes supplies.
But good routines can help cut down the number of decisions you’ll need to make each day and keep you on a healthy and happy pathway.
It’s normal to feel excited, but also a bit anxious about moving into your own place.
When you step into your new independent life, your parents, guardians, and other loved ones won’t be around to nudge you about managing your diabetes. And this can feel a little overwhelming.
You might be juggling a new job or studying, meeting new flatmates, or figuring out grocery shopping and meal prep. It can get a bit hectic and intense, so having a support system is key.

Find a late-night hours NDSS Access Point (usually a community pharmacy). Go to healthdirect to find a community pharmacy near you.
You can also call the NDSS Helpline 1800 637 700 and ask to speak to a diabetes health professional. They’re there to help you.
As you become more independent it’s a good time to check in with you diabetes health professionals about what these changes will mean for managing your diabetes.
It’s also a good time to refresh your diabetes management, so that you can make the best decisions for yourself based on the best information.

Whether you’ve been living with type 1 diabetes for most of your life or just for a short time, you will already know a lot about it.
Becoming more independent is a step up in responsibility, including managing the diabetes supplies you need.
It may take some time to adjust and plan ahead now that you don’t have a parent to remind you.

Stock up on necessary diabetes supplies like syringes, needles, batteries, spare insulin pens, blood glucose monitoring strips and glucose sensors if you are using CGM or Flash GM, and have a blood ketone meter and strips in your sick day action kit.
Keep a record of your basal insulin rate, insulin-to-carb ratio, and insulin sensitivities if you’re using an insulin pump.
Know how and where to dispose of used sharps such as pen needles.
For troubleshooting:

Will, 21 years

As a young person with type 1 diabetes, it’s really important to know if your blood glucose levels are within your target range. This helps both you and your diabetes health professionals to make sure your diabetes management is on track.
The HbA1c shows your average blood glucose levels over the past 10-12 weeks.
For most people with type 1 diabetes, the recommended HbA1c target is less than 7% (53 mmol/mol). But everyone is different, so your personal target might be different too. If you’re not sure about your HbA1c level or target, chat with your diabetes health professional about it.
If your last HbA1c showed a higher level than your target, it might be time to tweak your diabetes management. You might need to adjust your insulin doses or make some lifestyle changes. Remember, your diabetes health professional is your go-to person for ongoing support, personalised advice, and to explore the best options to help you manage your diabetes.


To stay on top of your health, other checks are needed through the year. This is usually done via an annual review with your GP, known as an annual cycle of care. The annual cycle of care is important as it helps pick up any issues early and helps keep your diabetes management on track.
Some of the checks done include blood pressure, glycated haenoglobin (or HbA1c), kidney function, eye health and feet check. Your GP will coordinate any referrals for review appointments with the relevant diabetes health professionals.
If you’re not sure what to do, or you can’t get your diabetes on track, call your diabetes health professional. You can also call the NDSS Helpline 1800 637 700 and ask to speak to a diabetes health professional. They’re there to help you.

Ky, 21 years
Eating well with diabetes doesn’t have to become a daunting task when you move out of home. In fact, nutrition recommendations for people living with diabetes is no different from what’s recommended for everyone else.
Eating nutritious foods and being active will be your best friends when it comes to managing your blood glucose levels and boosting your energy levels. By choosing nutritious options, you can still enjoy delicious meals and snacks while taking care of your body.

Meals don’t have to be complicated or time-consuming to be balanced. On the following pages, you will find plenty of breakfast, lunch and dinner meal ideas for inspiration. Feel free to pick, choose and swap to suit your taste and dietary requirements. Remember your portion size and amount of carbs may need to be adjusted to suit your individual needs. Speak to a dietitian for more information.

Avocado toast

Tuna pasta salad

Chicken nourish bowl
There are many types of eating plans that may be suitable for people with diabetes.
How you eat is up to you. When it comes to type 1 diabetes and eating well, some nutrition tips and recipe inspiration may help you work out what to eat each day, depending on your needs and food preferences.
Choose to drink water first. Limit sugary drinks such as soft drinks, cordials, energy drinks and flavoured milks.



Vegetables are a low-cost way of adding nutrients to your meal.
In the shop, pre-packaged vegetables are sometimes more expensive than bagging them yourself. Compare the unit price to see how much you are paying for plastic wrap.
Frozen vegetables can be as good as fresh vegetables. Buying frozen vegetables is also convenient and helps reduce food waste as they will not go off.

You can cut your shopping bill down by swapping animal protein (such as mince or steak) for plant-based protein (such as legumes) in your meals.
Did you know 65 grams (g) of animal protein is equal to 125 g of protein from legumes.
Legumes also provide an added benefit of giving your meals more fibre.
If you include snacks as part of your eating plan, try to have snacks from the five food groups.
If you prefer to purchase pre-made snacks from the supermarket, the FoodSwitch app can be a good tool to have on your phone. It’s an easy way to make sure you’re buying the best version of that snack.

It works by following these steps:



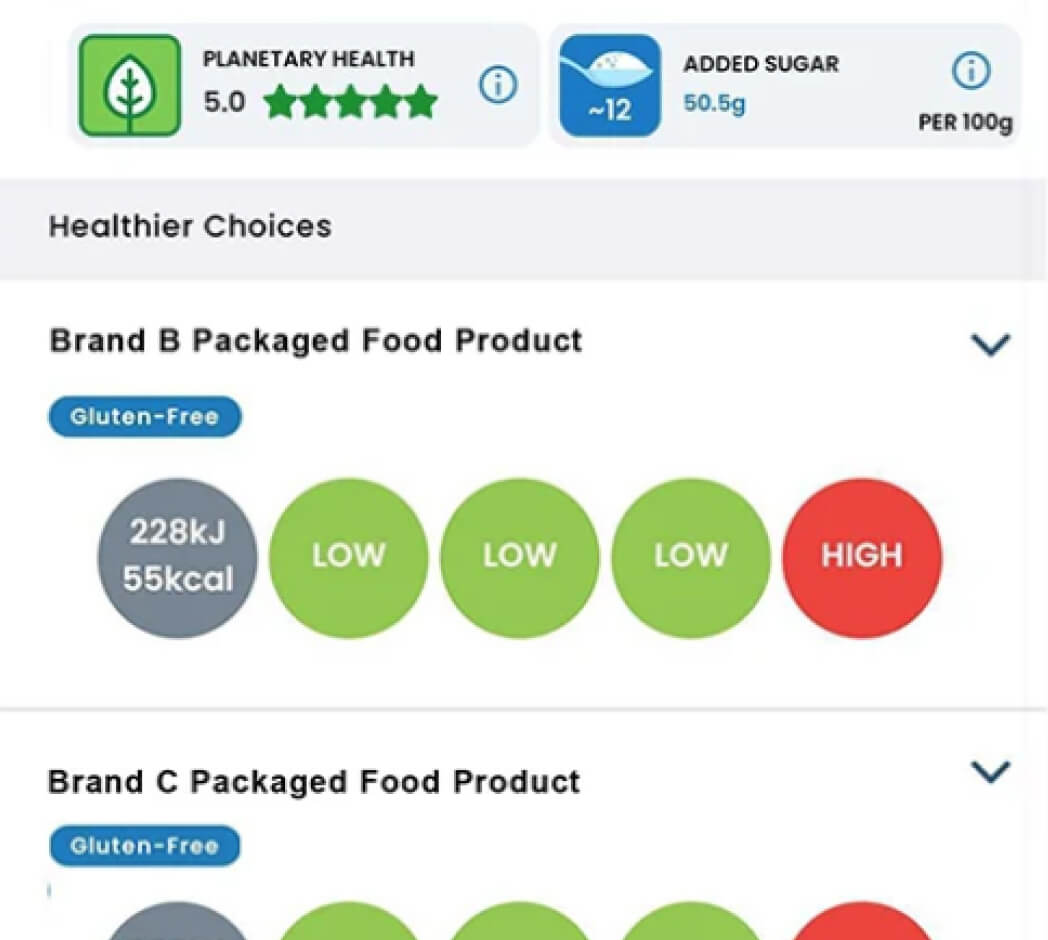
The app doesn’t provide information on fibre. Aim to choose foods that have 5 g or more of fibre per 100 g. You’ll find this information on the back of the food product in the nutritional information panel.
For more about label reading and the benefits of a fibre-fit eating pattern go to Eating and Drinking.





It’s important to talk to your diabetes health professionals about managing your diabetes when you’re eating out. They can help work out your insulin dosing based on your food choices.
For more information on Eating and drinking including:

Quiz
This information is intended as a guide only. It should not replace individual medical advice. If you have any concerns about your health, or further questions, you should contact your health professional.

Time is Up!

Time's up