The NDSS is administered by Diabetes Australia
- /
- Insulin
Now you’re living with type 1 diabetes, you would have started on insulin as soon as you were diagnosed. This is to replace the insulin your body no longer makes.
Insulin is an essential part of managing your diabetes and will help keep you feeling well.
Insulin is a hormone made by the pancreas. The pancreas is an organ in your body. The easiest way to describe insulin is as a key that unlocks the cells in the body to let in glucose to be used as fuel or energy.
Type 1 diabetes is an autoimmune condition where the person’s immune system attacks the cells in the pancreas that make insulin. Without insulin, glucose builds up in the bloodstream, leading to high glucose levels.
Not having any insulin will cause high blood glucose levels and make you wee a lot, feel tired and thirsty, and lose weight. It can also lead to you becoming seriously unwell with diabetic ketoacidosis (DKA). Replacing the insulin your body no longer makes with insulin injections or via an insulin pump is life saving when you have type 1 diabetes.

Everyone with type 1 diabetes needs to replace the insulin their body no longer makes. The insulin you inject, has the same effect as the insulin that was made by your pancreas. There are several ways to do this. You’ll be able to work with your diabetes health professionals to help you decide which method is best for you. It may be with an:
The method you chose may change in the future; especially as new technology becomes available.
Your diabetes doctor (endocrinologist, paediatrician, or other diabetes specialist) or diabetes nurse practitioner will work with you to plan the type and amount of insulin you need over the day. While there are different brands of insulin, they all fall into three groups.
A basal insulin is a long-acting insulin. It works slowly and is often described as a background insulin. Basal insulin works over 24-36 hours to keep your blood glucose level stable between meals and overnight. It should be injected at the same time each day but doesn’t need to be taken with food.
A bolus insulin is a rapid or short-acting insulin. It works quickly and helps balance your blood glucose level over 2-6 hours. Bolus insulin is given with a meal and sometimes with a snack. The dose is calculated based on the amount of carbohydrates (carbs) you will have and the blood glucose level. This is called the insulin to carb ratio (ICR).
Bolus insulin can also be used to correct a high blood glucose level.
A “mixed insulin” has a combination of a bolus and basal insulin. It’s usually injected once or twice a day.












Different sites may cause the insulin to work faster or slower depending on the type of insulin you use. This is the same if you’re using a syringe, insulin pen and pen needles, or an insulin pump.
Insulin is injected into the fatty (subcutaneous) layer under the skin. The more common sites used are the tummy (abdomen) and upper buttocks.
If using arms or thighs, it’s important to avoid injecting into the muscle. The insulin will be absorbed much faster in a muscle, increasing the risk of a hypo.
Talk to your diabetes health professional about which injection sites you can use.
It’s important to “rotate” injections within your chosen injection site. Lipohypertrophy is a firm, fatty lump that appears on the skin. It happens when injecting in roughly the same spot over a long period of time. This changes the appearance of the skin and can also affect how quickly insulin is absorbed.
If you find a fatty lump, avoid using the area until the lump is gone. Talk to your diabetes health professionals if you’re worried about your injection sites.
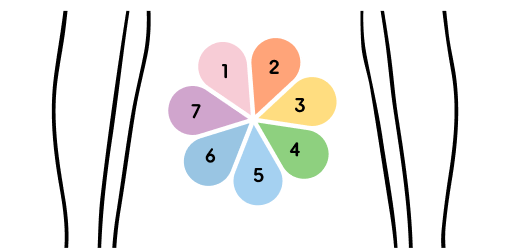
An easy way to rotate insulin injection sites is to imagine a flower shape on your stomach, like in this diagram. Use one petal of the flower each day of the week to inject insulin, with each injection being in a slightly different spot in that petal.
No one really likes having injections. The good news is that the pen needles and cannulas are now very fine, and generally, injections are pain free. Just in case, here are a few tips to reducing the pain.


Using a blunt needle can cause bruising and pain.
Top tip: Change your pen needle with every injection.
Some medication such as aspirin can cause bruising and bleeding.
Top tip: Apply pressure over the injection site with your fingers for 50 seconds after injecting.
Using cold insulin can cause stinging and pain.
Top tip: Use insulin at room temperature between 4-25 degrees Celsius.
Some insulins can cause burning or stinging when injected.
Top tip: Choose a slightly longer needle length, for example change from a 4mm to a 5 or 6 mm pen needle.
Getting anxious when having to inject?
Top tip: Find some relaxation techniques such as slow breathing.
An insulin pump is a programmable device, smaller than a smartphone. It uses rapid-acting insulin only. It’s connected through a small plastic cannula that sits under the skin. Most pumps use tubing to deliver the insulin from the pump to the person. But there is also a pump that is tubeless called a pod.
Pumps are programmed to automatically deliver the basal insulin in small amounts over 24 hours. Bolus insulin is given at mealtimes or when the blood glucose level is above the target range, with the press of a button.
If you decide to use a pump, your diabetes health professionals will:
There’s a lot to think about when deciding to use a pump.
Here’s a list for you to think about.
Using insulin, isn’t just learning to give an insulin injection. It’s also about finding out how to store it safely. You also need to know how to dispose of the used equipment.
Keep any insulin you are not using in the fridge. The ideal storage temperature is 2 to 6°C.
Keep your insulin out of direct sunlight in a cool cupboard or cooler bag.
If you leave insulin out of the fridge for 28 days or more throw it away as the insulin will have broken down.
Some insulins may need to be stored differently. Read the information that comes with it, or ask your diabetes health professionals for advice.

You will need to dispose of your used syringes, pen needles or used cannula and inserter in a safe way.
They’re called sharps because they puncture your skin.
Just throwing your sharps out in your general garbage, household recycling or public litter bins increases the risk of a needle stick injury. This may affect people who handle your garbage, the people around you or even children.
Your NDSS registration gives you access information, programs, support services and subsidised diabetes products through your local pharmacy.