The NDSS is administered by Diabetes Australia
Menu
- /
- Wellbeing
Looking after your mind is just as important as looking after your body. It’s okay to feel down, frustrated or fed up sometimes. The important thing to learn is the things you can do to feel better so you have more good days, than bad.
Living with type 1 diabetes can be like carrying around a box. Some days it’s easy; on others, it’s heavy and feels like two boxes instead of one. And then there are days it feels like the box has morphed into many boxes!
It’s okay to feel not okay about diabetes. It can be complicated, sometimes scary, and uncomfortable, and you never get a day off. Just because something worked once doesn’t necessarily mean it will work the next day. This can be hard because you might have done all the ‘right things’ yet still feel disappointed.
When you have one of these days, or the boxes are stacking up, be kind and patient with yourself.


Angie, 17 years

Run, swim or kick a ball with friends, punch a boxing bag, or go skateboarding. Exercise releases happy hormones that make you feel better.

If there’s one thing for sure, diabetes is something you always have to think about. Be kind and patient with yourself – don’t expect perfection.

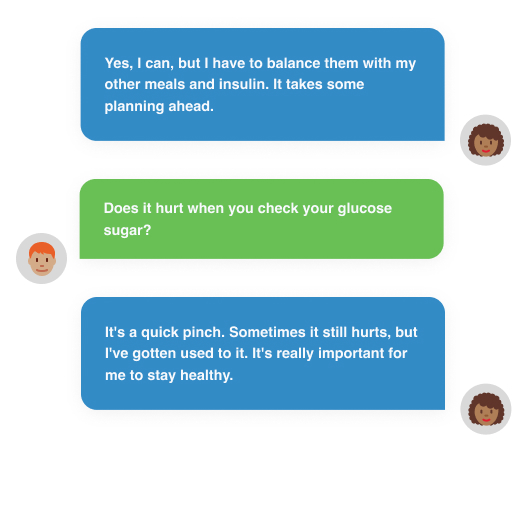
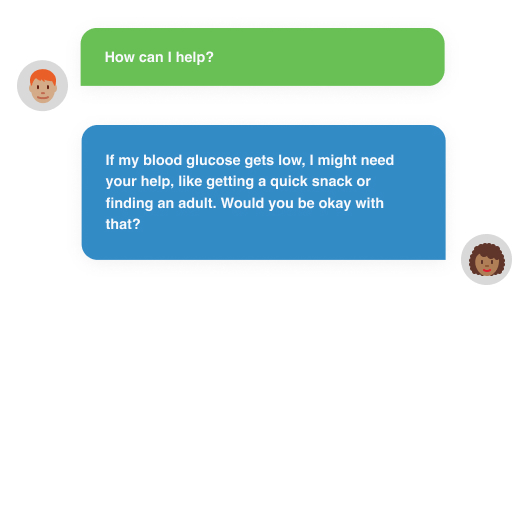
Sometimes you might feel mad, sad or fed up with diabetes. You might even feel like a human calculator every time you eat. For example, working out things like counting carbohydrates (carbs) or insulin doses. Talk to someone and tell them how you feel. Just saying it out loud can ease some of the bad feelings. Managing diabetes is a big deal; your friends and family will want to support you in any way they can. Ask your diabetes health professionals for help.

Living with diabetes is different for everyone. Having a chance to talk to other young people who also have diabetes can be really helpful. The NDSS and Diabetes Australia have day activities for kids. JDRF have programs that offer peer support and connection with those that have diabetes.


If managing diabetes feels too much, talk to a psychologist familiar with diabetes. They can help you find ways to adjust to the changes in your life. Ask your doctor or diabetes health professional for recommendations, or check out the Australian Psychological Society website at psychology.org.au.

Get support through a GP Mental Health Treatment Plan. This will give you a rebate on the cost of seeing a psychologist.


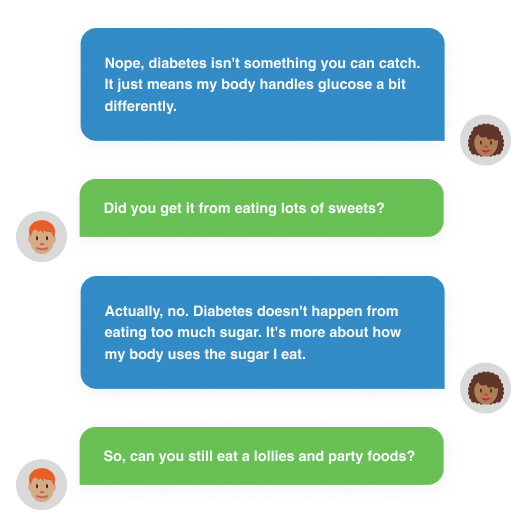
Some people are comfortable sharing with everyone about diabetes. They do school projects on it and even give a talk to the school.
Others might prefer to keep things a bit more private. That’s perfectly fine too!
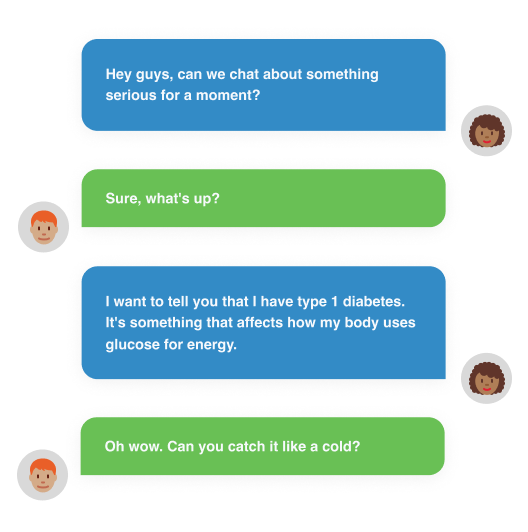
If you’re feeling a little nervous about telling your friends about your diabetes, that’s okay. Take a deep breath and think about who really needs to know right now. It could be your closest pals, your boss at your part-time job, or your coach and teammates at weekend sport.


Stress is part of life, but coping with diabetes on top of everything else can be a lot! Stress can raise blood glucose levels and increase other emotions such as anxiety, depression, tension, or anger. Learning how to manage stress is important for your diabetes and your wellbeing. Talk to someone about your worries and check in with your doctor or diabetes health professional about ways to cope with anxiety.
An Eating disorder treatment and management plan is for people who have been diagnosed with an eating disorder. It provides a rebate for sessions with a dietitian and a mental health professional.
Did you know people with type 1 diabetes make up to 180 extra decisions a day? No wonder this can lead to decision fatigue and stress.
People without diabetes don’t have to think about the many things you do. They don’t have to think about counting carbs, insulin doses, or the impact of what exercise, stress, illness or life will do to their blood glucose levels. But for you, it’s part of everyday life, every day, 7 days a week.
Managing type 1 diabetes can be challenging and frustrating. What works one day may not work the next.
Despite your best efforts, managing blood glucose levels can feel hard some days, especially during stress and illness. And in today’s fast-paced life, full of time pressures and competing priorities, it only adds to the pressure of managing type 1 diabetes. It’s common to think the numbers have to be “right”. If we do everything correctly, our blood glucose levels will be perfect, right?
It’s not so easy! Some days, diabetes seems to have a life of its own.
So what can we do? How can we build resilience during challenging times to keep on going?
When we’re stressed, our body releases the stress hormone cortisol. When cortisol is released, the following things happen:

Paula, diabetes health professional
Living with diabetes every day can be hard. It can lead to feelings of frustration, guilt, sadness, or worry. But it’s important to know you’re not alone if you feel this way. In fact these feelings are so common they even have a name for them, called diabetes distress.
Diabetes distress is the emotional burden of living with and managing diabetes. It’s important to recognise these feelings and get help early so they don’t start impacting daily life or lead to burnout.
Being angry, frustrated or feeling overwhelmed about managing your diabetes
Being worried about not taking proper care of your diabetes
Avoiding appointments or checking blood glucose levels
Making unhealthy food choices on a regular basis
Feeling alone and isolated or loss of interest in activities
Having unexplained blood glucose fluctuations
Being worried that you are ‘failing’ with your diabetes management
Feeling guilty when your diabetes management gets ‘off track’
If you feel this way, talk to your diabetes health professional or family. They can help you figure out ways to manage your feelings and prevent them from getting worse.
Burnout can happen if diabetes distress worsens or continues for a long time. Burnout is where a person is so emotionally exhausted and overwhelmed by the demands of their diabetes that they stop looking after their diabetes.
Diabetes burnout is very common. More than 3 out of 10 people with diabetes say that they feel burnt out by managing diabetes.
With so many extra decisions every day compared to someone not living with diabetes, it’s easy to understand why people with type 1 diabetes can develop diabetes burnout.
The risk of diabetes burnout is that people can become so emotionally exhausted by the demands of their diabetes that they stop looking after their diabetes.

Avoiding diabetes management activities such as monitoring your blood glucose levels, taking medications or insulin, or going to health professional appointments
Feeling alone and unsupported with your diabetes or being unable to cope with your feelings because they are overwhelming
Feel like diabetes is managing you rather than you’re managing your diabetes


Sometimes life gets in the way. And you may not be able to do all your usual activities to manage your diabetes or have perfect blood glucose levels every day. Don’t sweat it. Think of your blood glucose levels as “outside of your range for now” rather than as “good” or “bad”.
Checking your levels is not a “test” that you can pass or fail. It just gives you information to help you manage your diabetes.

No one expects you to manage your diabetes on your own! Share the load by talking. It’ll help reduce the stress. Talking about what it’s like for you to have diabetes to family, friends, teachers, or a diabetes health professional is part of the journey. You may feel like you’re the only one with diabetes, but you’re not alone.

It’s really important to get enough sleep. Sleep helps your body repair itself, stay healthy and feel good. The amount of sleep you need varies from person to person but also depends on age. Here is a general sleep guide:
Like many skills, looking after your wellbeing can take practice. Practising wellbeing self-care every day, whether you’re experiencing a ‘down day’ or not, can reduce how often you experience ‘down days’. This can help you build resilience for when you experience ‘down days’. Taking time each day to practice wellbeing self-care will help you make ‘deposits’ into your wellbeing account! In time, your wellbeing account will grow and help protect you from the effects of stress.
Anytime you feel stressed and want to feel calmer, try this research-backed tool!
You do it like this: a double inhale through the nose, and typically, the second one is shorter, but it is still really important, and then exhale long through the mouth.
Take 1, 2 or 3 sighs to bring your stress level down and feel calm.

Take time for yourself.
Have compassion for you.
Look at challenges from different angles.
Get active and share good habits with family and friends.
Talk to a friend.
Wellbeing quiz
This information is intended as a guide only. It should not replace individual medical advice. If you have any concerns about your health, or further questions, you should contact your health professional.

Time is Up!

Time's up


NDSS Helpline
1800 637 700
Call the NDSS Helpline for information about diabetes, programs, support services and subsidised diabetes products. Ask to speak to a diabetes educator or dieititan.

Head to Health
Head to health gives access to a range of mental health information, advice and treatment options. It can help you seek support in times of need, or when it is most convenient for you.





Everyday mindfulness

Guided meditations and lets you track your progress

Daily workouts that change everyday
A scientifically proven app to help young people improve sleep and build better mental health