The NDSS is administered by Diabetes Australia
Menu
- /
- Physical activity
Creating good habits is key to living your best life with diabetes.
Make room for regular physical activities, whether it’s hitting the gym, walking your dog, or showing off your skills on the field with friends.
Feel great and boost your confidence.
Make new friends.
Sleep like a champ.
Keep a healthy weight.

Try to be active everyday. Remember, this might be something you build up to achieving.


Being active for 60 minutes every day.

It comes down to what you enjoy doing. Anything is better than nothing. Think about bike riding, team sports, surfing, yoga, pilates, dancing, or strengthening exercises.
The ideal combination is exercise that increases your heart rate (cardio-based exercise) and works your muscles (strength-based exercise).
This will help your insulin work better and create more muscles which can store and take away the glucose from your bloodstream.

Check out scavenger hunt apps for some fun new ideas.
It’s easy to love your screens. Did you know that managing your screen time and moving more can actually be a game-changer for your health, happiness, and success?
Let’s dive into a super fun plan to help you get the most out of your screen time, manage your diabetes and feel more energised and active!

It’s important to know how much time you’re actually spending on screens each day. Use a screen time tracker app or your device’s built-in screen time monitor to keep track of your daily usage. You might be surprised at how quickly it adds up!

Now that you’ve a better idea of your screen time habits, it’s time to set some goals. Decide on a realistic limit for your daily screen time and document it in your online journal. Remember, limit your screen time to 2 hours per day, outside of screen-based activities for educational needs. The goal is to find a balance between screen time and other activities, so don’t be too hard on yourself.

Let’s make this fun by finding exciting activities to replace some of your screen time.
The possibilities are endless, so get creative and find what you love!


Playing competitive sports with type 1 diabetes can be challenging, but with the right tips, you can have fun and achieve in your favourite activities.
Keep in mind that everyone’s body responds differently to exercise, so you will need to work with your diabetes team to make a plan and adjust your activity, carbs, and insulin as needed.

When playing sports, you’re part of a team. Handling diabetes during sports involves another important team; your diabetes health professionals. They’ll guide and help you manage diabetes for your health and sports performance.
By working out how your body responds to different activities and using their advice, you’ll become a pro at tweaking activity, carbohydrates (carbs), and insulin to match your activity levels.

When packing your sports bag, don’t forget your diabetes kit.
Your diabetes kit should have:

Make sure the coach knows about your diabetes, what to look out for, and how to deal with any problems.
Give your coach written instructions about signs of hypoglycaemia (a hypo) and how to treat it, where your diabetes kit is, and when and how to give glucagon if needed. Make sure they know when to call 000 and how to reach your parents or carer in an emergency.

Your blood glucose targets before and during exercise should be based on your needs. Your diabetes health professionals can help you set goals depending on the type and length of exercise and your situation.
Usually a blood glucose level of between 7 and 10 mmol/L is considered a sweet spot for exercise.
Check your blood glucose before, during, and after exercise. This helps you and your diabetes health professionals understand how your body reacts to different types of physical activity and sport. Your diabetes health professionals can help you fine-tune your insulin, activity and carb intake for top performance.

If your blood glucose level is under
4 mmol/L, this is a hypo. Treat it and stop exercising until your blood glucose is in the target range.
If your blood glucose level before exercise are between 4 and 7 mmol/L, you may need some extra carbs before, during or after exercise.
Delayed onset hypos can happen up to 24 hours after exercise. This is because your muscles keep taking up glucose while they recover. Check your blood glucose before bed and overnight, especially if you’ve exercised a lot in the afternoon. Everyone is different and reactions to exercise vary from person to person. Blood glucose level can change depending on the type of exercise, your fitness and how you manage your diabetes. Ask your diabetes health professionals for advice about how you can reduce your risk of hypos when you exercise.

Check for ketones if your blood glucose level is higher than 15 mmol/L before or during exercise.
If you have blood ketones between 0.6-1.5 mmol/L you may need to stop or delay exercise and have a correction dose of insulin to help clear the ketones. You will have to wait 15-60 minutes to reassess if your blood glucose and ketone levels have normalised before starting exercise.
If your blood ketones are higher than 1.5 mmol/L, you must not exercise.
Exercising when your blood glucose levels are high and you have ketones can be dangerous. This is because your muscles don’t have enough insulin to use glucose for energy. You could be at risk of developing DKA (diabetic ketoacidosis). Ask your diabetes health professionals how you should best manage exercise if your blood glucose is outside your target range or you have ketones.
Remember, with the right planning, support, and determination, you can excel in any sports while managing your type 1 diabetes.
Stay active, stay healthy, and aim high!
These help raise your blood glucose level quickly. Pack 2 or 3 of these in your kit:
After treating a hypo, you might need a snack to keep your blood glucose steady. Here are some ideas:

Gary Hall Jr.
American swimming star and 10-time Olympic medalist
Too much screen time is not healthy.
Try to do 2 hours or less per day of screen time. Break up long periods of sitting as often as possible.
Sleep is super important!
Try to go to bed and wake up at the same time each day (even on weekends). If you’re aged under 13 you’ll need 9-11 hours per night. If you’re aged 14-17 you’ll need 8-10 hours per night.
Everyone feels stressed sometimes.
But did you know stress can impact diabetes? Stress releases hormones that increase blood glucose levels. Exercise is a two-for-one deal. It helps us feel less stressed, and reduces blood glucose levels at the same time!
This is an open access article under the terms of the Creative Commons Attribution-NonCommercial License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited and is not used for commercial purposes. © 2022 The Authors. Pediatric Diabetes published by John Wiley & Sons Ltd
This is an open access article under the terms of the Creative Commons Attribution-NonCommercial License, which permits use, distribution and reproduction in any medium, provided the original work is properly cited and is not used for commercial purposes. © 2022 The Authors. Pediatric Diabetes published by John Wiley & Sons Ltd

This exercise is still good for you as it builds more muscle which stores more glucose. Your blood glucose level will usually go back down in 1 to 2 hours.
Attention: Watch out for late onset of hypos.

Think of your muscles like a sponge, soaking up and using the glucose in your bloodstream every time you work your muscles.
Attention: You may need extra carbs depending on your blood glucose levels and the amount of insulin in your body (on board).

Blood glucose levels usually remain steady. Activities like team sports tend to stop and start, combining high and low intensity activity. These types of sports often result in stable blood glucose levels compared to continuous aerobic activity such as cycling, going for a run, swimming laps.
Attention: Watch out for late onset hypos. Remember, you may also need to have carbs during these types activities.
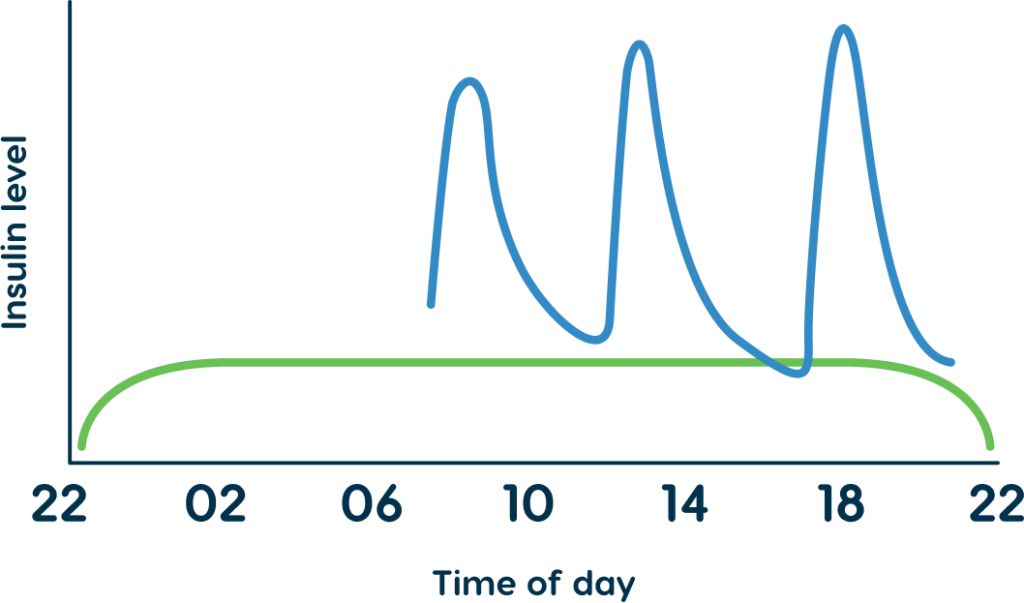
Avoid exercising during the peak of insulin action. You could do this by planning exercise sessions to be:
This does require some advanced planning and may not work out if you’re training for a sport or can’t change your exercise times. If that is the case you could look at:
Exercise type and intensity:
Exercise duration
The time of day of exercise
Insulin use before exercise including:
Carbs and fluid needs during exercise

It’s important to work with your diabetes health professionals to develop an exercise plan. An exercise plan should include guidance about how and when to adjust insulin and tips about carbs in meals and snacks. This is important for staying safe, but it will also help getting the most out of exercise.
Don’t forget to review the plan regularly to adjust for changing needs such as growth and a new insulin regimen.